The search term “Emergency dentist near me” gets almost 4000 searches in the local area per month, so we know that people looking for an emergency dentist and that they need information about treatments and options available.
We have broken this article on emergency dental treatments down into a few headings:
- Teeth which have come out completely.
- Loose teeth.
- Broken teeth.
- Tooth abscesses.
1. Teeth which have come out completely
What to do if the tooth comes out completely
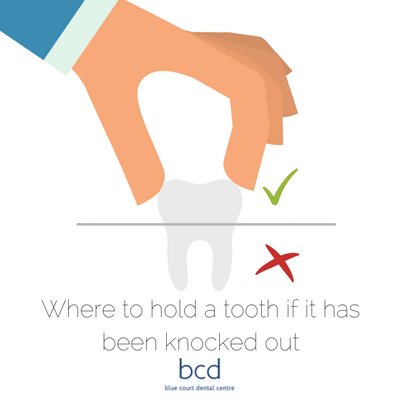
If the tooth has come out completely you may be able to replace it so long as it is not damaged. If there are still blood vessels or nerves attached do your best to keep these intact and only hold the tooth by the crown section and not the roots.
If you can, gently place the tooth back into the socket ensuring it is the right way round. Only do this if the tooth is completely clean and hasn’t been in contact with the ground.
If the tooth has been in contact with the ground place it into a clean (ideally sterile) plastic bag with some milk and take it with you to your dentist or accident and emergency at the local hospital.
If the socket is bleeding profusely then gently bite down onto a soft piece of gauze, when the bleeding subsides don’t immediately remove the gauze as this could dislodge the blood clot and the bleeding could start again. Alternatively use a cold teabag, it has been shown that the tea contains substances which can help to reduce the amount of bleeding.
Do teeth grow back in adults?
Unfortunately not. Once your baby/deciduous teeth have fallen out you only get one set of permanent teeth. The only teeth which may grow after this initial set have come through are the very last molars or wisdom teeth.
2.Loose teeth
Can a loose tooth become tight again?
If the looseness of the tooth has been caused by gum disease then yes, if the gum disease is treated and the problem resolved then the tooth can tighten up again. This shows the importance of the early treatment of gum disease and how the situation can be saved if caught early.
3.Broken teeth
Is a chipped tooth an emergency?
A chipped tooth is only an emergency if either the tooth is bleeding or the gum surrounding the tooth is bleeding and won’t stop. If the tooth has chipped and there is no pain or bleeding then this would not normally be considered a dental emergency, you should however make an appointment to see the dentist as soon as possible to rebuild the tooth if required.
Can a chipped tooth heal itself?
Amazingly, yes, a chipped tooth can heal itself but it won’t rebuild itself. If the tooth chips and the softer underlying dentine has become exposed the tooth will react to this and create what is known as secondary dentine. This secondary dentine is often much darker but is also harder and will protect the softer underlying tooth. If you want the full contour of the chipped tooth to be restored then the only way to do this is to visit your dentist who will then use dental bonding or possibly veneers or a crown.
How to fix a chipped tooth
A chipped tooth can only be fixed by your dentist. If the chip is small then they may use dental bonding to rebuild the full contour of the tooth. If the chip is significant then dental bonding may not be adequate and a full dental crown or veneer can then be used. This may require a small amount of reduction of the healthy tooth structure in some instances.
4.Tooth abscesses
Is an abscess a dental emergency?
Yes. an abscess is a buildup of pus from an infection around the tooth. It is characterised by significant swelling, redness and pain. An abscess will not go away on its own and in extreme circumstances can spread to other parts of the body and make you ill.
What helps a tooth abscess?
If you have a tooth abscess then we recommend you contact your emergency dentist as soon as possible, whilst you are waiting to see them you can reduce the pain by rinsing your mouth with warm salt water, this is particularly effective if the abscesses caused by gum infection. Saltwater can help to remove bacteria from the infected area.
We also recommend:
- Taking recommended doses of over-the-counter painkillers.
- Avoiding particularly hot or cold food and drinks as it may make the pain worse.
- Eating on the opposite side of your mouth.
- Using a softer toothbrush than you would normally and don’t floss around the affected area until it has been seen by a dentist.
Please note, these are all temporary solutions and you will need to see a dentist to get the abscessed sorted.
Dr Nishan Dixit
Latest posts by Dr Nishan Dixit (see all)
- Dr Dixit is the new President of British Academy of Cosmetic Dentistry - 28 May 2020
- Does Invisalign hurt? - 9 March 2020
- How Long Does Invisalign Take? - 27 February 2020


 Gum disease, which includes periodontal disease, is inflammation and infection that destroys the tissues that support the teeth, including the gums, the periodontal ligaments and the tooth sockets (alveolar bone). Gum disease affects more than half of the adult population with natural teeth. It can be treated by a dentist or hygienist and in the early stages the effects can be reversed. There are two main types of gum disease:
Gum disease, which includes periodontal disease, is inflammation and infection that destroys the tissues that support the teeth, including the gums, the periodontal ligaments and the tooth sockets (alveolar bone). Gum disease affects more than half of the adult population with natural teeth. It can be treated by a dentist or hygienist and in the early stages the effects can be reversed. There are two main types of gum disease: